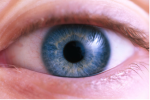
 One of the many healing properties attributed to breast milk is the ability to cure eye infections such as ‘pink eye’ — conjunctivitis — or ‘sticky eye’ — a gooey discharge that often accompanies conjunctival inflammation. Conjunctivitis is a common condition that rarely requires treatment, usually clearing up by itself within a week or two. For newborns, however, it can occasionally be quite serious, so ensuring it is properly treated is very important. For everyone else, it can be irritating and unpleasant, so any way of reducing the length of the infection is naturally welcome. Can breast milk really provide any relief?
One of the many healing properties attributed to breast milk is the ability to cure eye infections such as ‘pink eye’ — conjunctivitis — or ‘sticky eye’ — a gooey discharge that often accompanies conjunctival inflammation. Conjunctivitis is a common condition that rarely requires treatment, usually clearing up by itself within a week or two. For newborns, however, it can occasionally be quite serious, so ensuring it is properly treated is very important. For everyone else, it can be irritating and unpleasant, so any way of reducing the length of the infection is naturally welcome. Can breast milk really provide any relief?
A study in a hospital in New Delhi, India, examined the effect that routinely applying colostrum to babies’ eyes had on the likelihood of them developing an eye infection1. On one hospital wing, mothers were asked to put a drop of colostrum in their babies’ eyes three times a day; on another wing, mothers were asked not to apply anything. The infection rate was much lower in the babies who received colostrum: only 3 out of 51 babies in this group (6%) developed an infection, compared to 26 out of 72 in the control group (35%).
At first glance, this seems like a convincing result for colostrum, but a closer examination of the figures indicates this isn’t necessarily the case. The normal neonatal eye infection rate recorded at the hospital was just over 5% – roughly the same as the one recorded in the colostrum group. Rather than infection rates going down in the babies who received colostrum, it seems they went up – considerably – in those who didn’t. This may have occurred because the normal practice of wiping eyes with a sterile swab just after birth was abandoned during the study. Fewer babies in the study group may have got infections simply because their eyes were rinsed, not necessarily because it was with colostrum.
There is other evidence that breast milk could help ease the symptoms of conjunctivitis, however: in vitro tests show that colostrum, and to a much lesser extent mature breast milk, can potentially combat some of the bacteria known to cause neonatal eye infections2,3, and another study provides evidence that it does seem to be an effective treatment for eye infections in young babies4. At a hospital in Spain, babies diagnosed with neonatal sticky eye were treated either with antibiotics or breast milk. Babies treated with breast milk generally recovered much faster: 26 out of 45 (57%) of those receiving milk had recovered after 30 days, compared with 3 out of 20 (15%) of those receiving antibiotics. Whilst this does not provide conclusive evidence that breast milk is the optimal treatment for eye infections in newborns, the study’s results were deemed sufficiently encouraging to switch from antibiotic drops to breast milk at the hospital where it took place.
So does this limited evidence that breast milk can treat some neonatal eye infections mean it can be used to treat infections in older children, or even adults? Whether breast milk would have a beneficial effect is not clear: its antibacterial properties mean that it may help to clear up an infection caused by certain types of bacteria, but not necessarily one resulting from an allergy or a virus. Having said this, there is, of course, no harm in trying the breast milk option. If you’re currently nursing, it’s simple and free, and whilst it may not get rid of the symptoms, it almost certainly won’t make them any worse.
 Many years ago, breast milk was thought to be sterile. While this is far from being the case (it actually contains all manner of germs
Many years ago, breast milk was thought to be sterile. While this is far from being the case (it actually contains all manner of germs According to the
According to the 